To our PSC Community: Learn the Difference Between PSC and PBC
Read this news release: “PSC Partners Seeking a Cure Surpasses 1,000 Patients in International Registry and Discovers Unexpected Misdiagnoses”
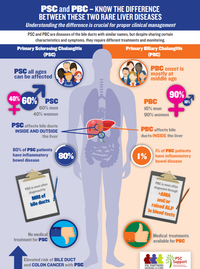
The international community of the bile duct disease PBC (formerly known as primary biliary cirrhosis) has changed the disease name to primary biliary cholangitis. PSC Partners Seeking a Cure and PSC Support in the UK believe this name change presents an opportunity to educate our global PSC community.
Although PSC and PBC share certain symptoms and characteristics, they require different treatment and monitoring to ensure patient safety. Our aim is to highlight the differences between the two conditions, so that PSC and PBC patients alike may avoid the dangerous and detrimental effects of an inaccurate diagnosis.
On January 21, 2017, Dr. Christopher Bowlus, Co-Chair of the PSC Partners Scientific and Medical Advisory Committee (SMAC) and scientific head of PSC Partners’ Patient Registry, gave a presentation on PSC and PBC at the University of California, Davis. The meeting focused on the basics of PSC and PBC, as well as current treatment options and clinical trials available for both conditions. Dr. Bowlus specializes in researching and treating autoimmune liver diseases, with a particular emphasis on PSC, PBC, and AIH. See the slides from this presentation.
Why you need to understand the difference between PSC and PBC?
- PSC and PBC sound like the same disease.
- Focusing solely on the names of these conditions, both are “primary” diseases (not secondary, that is, not caused by another condition).
- Both are “biliary,” that is, diseases of the bile ducts.
- Following the name change for PBC, both are now characterized by the term “cholangitis.”
- However, the two diseases are not the same, despite sharing certain similar characteristics and symptoms. Each condition creates different needs among patients, and each requires different treatments and monitoring.
We have witnessed errors caused by the similarities in the name of the two diseases. We encourage you and your care providers to be informed about the differences between the two diseases. Our two organizations (PSC Partners Seeking a Cure in the US and PSC Support in the United Kingdom) have worked together with hepatologists who also see the importance of educating our patients on this issue.
Why the name change?
- PBC patients have justifiably wanted to change the disease name to avoid the stigma of the term cirrhosis.
- By changing cirrhosis to cholangitis, there is no longer a misconception that PBC is caused by alcohol overuse.
- Additionally, 80 percent of PBC patients no longer progress to cirrhosis.
- Unlike most PSC patients, a large number of PBC patients respond to ursodeoxycholic acid (UDCA), which, in their case, slows down disease progression.
- The term cirrhosis in the disease name no longer reflects the reality of the disease.
What specific problems might the confusion between PBC and PSC cause?
PSC patients are not always treated by experienced hepatologists. As we know, some gastroenterologists and primary care physicians may never have treated a PSC patient and do not know the risks associated with PSC. In many cases, a patient with a rare disease like PSC will not have access to a hepatologist who specializes in PSC or is involved in PSC research. Knowing the difference between the two diseases is important because PSC and PBC create different clinical needs.
Difference Between PSC and PBC
- One significant difference between the two diseases is that PSC is considered a premalignant disease, which presents an increased risk of colon and bile duct cancers. Accordingly, PSC patients need to be closely monitored for cancer and for assessing their response to ursodeoxycholic acid (UDCA). PBC has no such increased risks. An erroneous diagnosis that results in neglect of regular monitoring could have disastrous results for PSC patients.
- A second difference between PSC and PBC is the way the two diseases manifest in patients. PSC affects individual patients differently; there is no single disease course, and there are many factors to be considered with PSC. Whereas PSC has several unknowns and many unmet needs, PBC is not as multilayered.
- Furthermore, the World Health Organization (WHO) classifies and provides different codes for each disease. PSC and PBC may be confused in disease coding for insurance or for medication purposes. Whether you are a patient or a caregiver, please make sure you are aware of the potential for error. The ICD-10-CM Code for PSC is K83.01.
The most critical points that identify and differentiate the two diseases are represented in the table below.
Table 1: Similarities and differences between PSC and PBC
| FEATURE | PSC – PRIMARY SCLEROSING CHOLANGITIS | PBC – PRIMARY BILIARY CHOLANGITIS (COMMONLY STILL REFERRED TO AS PRIMARY BILIARY CIRRHOSIS) |
|---|---|---|
| Site of disease involvement | Bile ducts inside and outside the liver; however in small duct PSC (10-15% of patients) only the small ducts inside the liver are affected | Small bile ducts inside the liver only |
| Mode of diagnosis | Usually by MRI of bile ducts. Occasionally liver biopsy or ERCP is needed | Two of the following: Raised ALP, positive disease specific antibodies (AMA), diagnostic liver biopsy. |
| Associated with increased risk of bile duct cancer and colon cancer | Yes | No |
| Response to ursodeoxycholic acid (UDCA) | Improves liver blood tests in some patients; not conclusively proven to slow disease progression | Associated with improved prognosis in those individuals who respond well to UDCA |
| Co-existing inflammatory bowel disease (IBD) | Around 80% of patients have IBD – mostly colitis | Very rare and not characteristic; around 1% |
| Common symptoms in early disease | Itching, fatigue, abdominal pain, cholangitis flares | Itching, fatigue, dry eyes and mouth, abdominal pain |
| Gender predominance | 60% men, 40% women | 90% women, 10% men |
| Average age at diagnosis | Any age; mostly around 40 years | 75% are affected in middle age (>45 years old) |
| Associated with excess alcohol consumption | No | No |
| Associated with smoking history | Most often non-smokers | Associated with a history of smoking |
References and Further Reading
- EASL Clinical Practice Guidelines: management of cholestatic liver diseases. J Hepatol 2009;51:237–67. doi:10.1016/j.jhep.2009.04.009
- Hirschfield GM, Karlsen TH, Lindor KD, et al. Primary sclerosing cholangitis. Lancet 2013;382:1587–99. doi:10.1016/S0140-6736(13)60096-3
- Trivedi PJ, Corpechot C, Pares A, et al. Risk Stratification in autoimmune cholestatic liver diseases: Opportunities for clinicians and trialists. Hepatology 2015;:n/a – n/a. doi:10.1002/hep.28128
- Boonstra K, Weersma RK, van Erpecum KJ, et al. Population-based epidemiology, malignancy risk, and outcome of primary sclerosing cholangitis. Hepatology 2013;58:2045–55. doi:10.1002/hep.26565
- Trivedi PJ, Hirschfield GM. Treatment of autoimmune liver disease: current and future therapeutic options. Ther Adv Chronic Dis 2013;4:119–41. doi:10.1177/2040622313478646
- Hirschfield GM, Gershwin ME. The immunobiology and pathophysiology of primary biliary cirrhosis. Annu Rev Pathol2013;8:303–30. doi:10.1146/annurev-pathol-020712-164014
- Floreani A, Franceschet I, Cazzagon N, et al. Extrahepatic autoimmune conditions associated with primary biliary cirrhosis. Clin Rev Allergy Immunol 2015;48:192–7. doi:10.1007/s12016-014-8427-x
- Corpechot C, Gaouar F, Chrétien Y, et al. Smoking as an independent risk factor of liver fibrosis in primary biliary cirrhosis. J Hepatol. 2012 Jan;56(1):218-24. doi: 10.1016/j.jhep.2011.03.031. Epub 2011 May 19.
- Juran BD, Lazaridis KN. Environmental factors in primary biliary cirrhosis. Semin Liver Dis. 2014 Aug;34(3):265-72. doi: 10.1055/s-0034-1383726. Epub 2014 Jul 24.
Acknowledgements
PSC Partners Seeking a Cure and PSC Support would like to thank Professor Gideon Hirschfield and Dr. Palak Trivedi for their involvement in helping us provide the following concise comparison between PSC and PBC.
Gideon Hirschfield, Professor/Consultant Hepatologist University of Birmingham/University Hospitals Birmingham
Dr. Palak Trivedi, Academic Clinical Lecturer and SPR in Hepatology and Gastroenterology NIHR Centre for Liver Research; University of Birmingham
Support for this project has been provided via a grant from Intercept Pharmaceuticals, Inc.
Complete your profile and join PSC Partners Seeking a Cure in advancing PSC research towards a cure. Find information about clinical trials.